Standard v high intensity supports price limits
November 2019
Issues Paper |
||||
|---|---|---|---|---|
The National Disability Insurance Agency (NDIA) has released this Issues Paper to assist individuals and organisations to prepare submissions to the Annual Price Review 2020-21. Individuals and organisations should not feel that they are restricted to comment only on matters raised in the Issues Paper. The NDIA wishes to receive information and comment on issues which individuals and organisations consider relevant to the Review’s terms of reference. Key dateSubmissions can be lodged
Contacts |
4. Price limits for group-based core supports 16
6. Plan Management Supports 22
8. Costs in outer regional areas 30
Terms that we use:
Introduction
No regulation (deregulated markets): this is typically used in cases where markets are highly competitive – for example, transport.
The imposition of price limits: this represents a maximum allowable price payable by participants for types of supports. This approach is used in a significant number of markets, which are still developing and growing, such as those for attendant care.
Terms of Reference
Review the price control framework to increase flexibility for participants and reduce administrative burdens for providers (see Chapter 2);
Review the price control framework for core supports, by examining:
how price limits for therapy supports should be adjusted annually, given the outcomes of the Review of Therapy Pricing Arrangements;
whether different price limits might be appropriate for different times of the day, or days of the week, for some capacity building supports, including for therapists, therapy assistants and for capacity building supports delivered by disability support workers; and
a loading should be applied to price limits and plan funding amounts in outer regional areas to account for the higher cost of service delivery, if any, in those areas (see Chapter 8);
Re-examine current billing arrangements, including:
In framing its recommendations, the Review will be cognisant of the objects and principles of the NDIS, including that the NDIS should:
Support the independence and social and economic participation of people with disability;
Be financially sustainable.
Timeline of the Review
The Review will commence in November 2019 and deliver updates and recommendations to the NDIA’s Pricing Reference Group and Board, for implementation from 1 July 2020. The Review will consult widely, undertaking stakeholder visits, workshops, and invitation of submissions and comments from all stakeholders.
| Date | Activity |
|---|---|
| November 2019 | Release of Issues Paper and call for submissions |
| November 2019 to February 2020 | |
| February 2020 | Release of preliminary findings of the Annual Temporary Transformation Payment Financial Benchmarking Study |
| March 2020 | Public submissions |
| By 31 May 2020 | |
| June 2020 | Release of final prices, immediately after the Fair Work Commission’s Minimum Wage Decision |
| 1 July 2020 | Implementation of new arrangements |
How you can contribute to this stage of the Review
This issues paper intends to assist you to prepare a submission to the Review. It sets out some of the issues and questions the Review has identified at this stage of the NDIS transition. You do not need to comment on every issue raised in this paper and you are free to raise any other issues or ideas that are relevant to the terms of reference.
The NDIA has listed several questions on the sections and topics under review. However, all stakeholders (providers, peak bodies, participants, advocates and others) may respond to points not covered by these questions or any other points they would like the NDIA to consider as part of the Review. The NDIA is especially interested in hearing from participants about any improvements that they might like to suggest to the NDIS Price Guide and Support Catalogue and the NDIS pricing arrangements.
Price controls for group supports;
Billing rules;
Any information that you consider to be of a confidential nature should be clearly marked or identified as confidential. The NDIA will not disclose such confidential information to third parties without first providing you with notice of its intention to do so, such as where it is compelled to do so by law.
Submissions may be lodged via email or post. Details can be found on page 2 of this Paper.
Increasing flexibility and reducing administration
Equally, the Agency must ensure that participants are fully informed and empowered to achieve maximum flexibility to use their budgets to meet their goals as they see fit.
The Annual Price Review 2020-21 is seeking the views of stakeholders on this topic and on any other issues that stakeholders wish to raise.
Is there scope for changes in the price controls framework that would give participants greater discretion over use of their budgets – without substantially increasing costs to providers?
Other issues
Price limits for 1:1 core supports
Current arrangements
Price limits also vary according to whether the worker is permitted to sleep when they are not delivering the support. There is a separate set of price limits for Night-time Sleepover Supports.
For supports where the worker is not permitted to sleep when they are not delivering the support, price limits also vary depending on the time of day and day of week that the support is delivered. There are different price limits for Public Holiday Supports, Saturday Supports, Sunday Supports, Weekday Daytime Supports, Weekday Afternoon Supports and Weekday Active Overnight Supports.
| TTP Price Limits (per hour) | Standard Intensity Supports | High Intensity Supports - Level 1 (Standard) | High Intensity Supports – Level 2 (High Intensity) | High Intensity Supports – Level 3 (Very High Intensity) |
|---|---|---|---|---|
| Weekday Daytime | $56.81 | $56.81 | $61.11 | $64.00 |
| Weekday Afternoon | $62.69 | $62.69 | $67.44 | $70.61 |
| Weekday Night | $63.85 | $63.85 | $68.69 | $71.92 |
| Saturday | $78.14 | $78.14 | $84.08 | $88.03 |
| Sunday | $101.61 | $101.61 | $109.32 | $114.46 |
| Public Holiday | $127.21 | $127.21 | $136.84 | $143.29 |
Standard v High Intensity Supports Price Limits
Daily Activities and Community Participation 1:1 supports delivered by DSWs are either Standard Intensity Supports or High Intensity Supports.
A support is considered a High Intensity Support if the participant requires assistance from a DSW with additional qualifications and experience relevant to the participant’s complex needs. The high intensity price limits may be considered when:
Definition of Time of Day and Day of Week
Every 1:1 DSW support is either:
(Note – The price limits for the Night-Time Sleepover supports are calculated as the sum of the Night-Time Sleepover allowance specified in section 25.7(d) of the SCHADS Award plus 3.5 times the relevant hourly price limit for Weekday Active Overnight Supports. The support includes the first two hours of work by the DSW if they have to work during the sleepover.)
A Public Holiday Support – any support to an individual participant that starts and ends between midnight on the night prior to a Public Holiday and midnight of that Public Holiday (unless that support is a Night-time Sleepover Support).
A Weekday Active Overnight Support – any support to an individual participant that commences at or before midnight on a weekday and finishes after midnight on that weekday, or commences before 6:00 am on a weekday and finishes on that weekday (unless that support is a Public Holiday Support or a Night-time Sleepover Support).
DSW Cost Model Assumptions
The NDIA has recently released a paper that sets out the methodology and assumptions that underpin its price limits for daily activities and community participation supports - see NDIS Cost Model for Disability Support Workers (NDIS DSW Cost Model).
Utilisation costs, as not all the DSW’s work hours are billable hours.
The costs of employing the DSW’s supervisor, including
Overheads; and
Pre-tax margin.
Issues
Whether the provision for overheads are adequate?
The Annual Price Review 2020-21 is seeking the views of stakeholders on these issues and on any other issues that stakeholders wish to raise.
Time of Day and Day of Week
Is it easy to determine whether the Public Holiday, Saturday, Sunday, Weekday Daytime, Weekday Afternoon or Weekday Night price limit applies to a given support? If not, how can this be made clearer?
In the DSW Cost Model, the supervision ratio refers to the ratio of disability care workers to direct supervisors, measured on a Full Time Equivalent (FTE) basis. Are the supervision ratio assumptions in the DSW Cost Model appropriate? If not, what not and what evidence?
Currently the DSW Cost Model makes the same assumptions about the mix of casual and permanent staff, utilisation and supervision ratios for every day of the week, and for all level of workers. Is this reasonable? If not, how should they be modified and why?
In the DSW Cost Model, margin refers to the excess of revenue (from the NDIS) over expenditure on the delivery of NDIS supports. What was the level of your margin in 2018-19 expressed as a percentage of all expenditure on the delivery of NDIS supports?
Are there any other issues with the price limits for 1:1 core supports or with the assumptions in the DSW Cost Model?
Price limits for group-based core supports
Current arrangements
Community-Based Group Supports
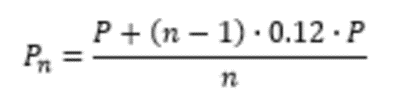
For each additional person in the group (after the first) an additional 12 per cent of the 1:1 price limit (essentially seven minutes) is added to the price limit. This reflects the time that the provider may need to spend writing a report on each participant in the group after the group has finished. Because of this built-in loading, providers of group based supports are not permitted to bill for non-face-to-face time. For 1:1 supports, non-face-to-face activities are part of delivering a specific disability support to that participant (rather than a general activity such as enrolment, administration or staff rostering).
Centre-Based Group Supports
Issues
An alternative approach would be for the base price for 1:n supports to be calculated as a simple proportion (1/n) of the base price of 1:1 supports but allow providers to bill for any non-face-to-face supports that they actually provided.
Some stakeholders have also expressed concerns that the capital allowance is too small and should vary according to the quality of the infrastructure being used to deliver the services. Conversely, other stakeholders have expressed concerns that the capital allowance is too large and provides an unintended incentive for centre-based supports.
Are these additional costs best dealt with:
a) Developing a separate DSW Cost Model for Group-Based Supports with different utilisation, supervision and overhead assumptions. If this is the preferred approach then what different assumptions should be made with respect to these key variables and why?
Other issues
Are there any other issues with the price limits for group based core supports?
Capacity Building Supports
Current arrangements
Finding and Keeping a Job – employment-related support, training and assessments that help a participant find and keep a job;
Improved Relationships – support to help a participant develop positive behaviours and interact with others;
Capacity building supports fall into two broad categories:
Therapy supports, including Early Intervention Supports for Early Childhood (ECEI) supports – these supports are delivered by the following registration groups: Therapeutic Supports (0128); Early Intervention Supports for Early Childhood (0118); Community Nursing Care (0114); Customised Prosthetics (0135); Exercise Physiology & Personal Well-being Activities (0126); and Specialist Positive Behaviour Support (0110); and
Issues
Whether different price limits might be appropriate for different times of the day, or days of the week, for some capacity building supports, including for therapy assistants and capacity building supports delivered by disability support workers?
Whether therapists and other capacity-building providers should be able to recover the costs of consumables provided to participants as part of a support? Currently, if providers of capacity building supports also want to claim for the cost of any consumables used in the delivery of the support then they are also required to register for the relevant assistive technology and equipment registration group. Some stakeholders have argued that providers of therapy and other capacity building supports should be able to recover the costs of consumables provided to the participant as part of the primary support.
Are the current price limits for capacity building supports adequate? If not, why not? Please provide evidence. How should the National Disability Insurance Agency (NDIA) determine price limits for non-therapy capacity building supports?
Should different price limits be introduced for capacity building supports delivered at different times of the day and days of the week, in line with the arrangements for core supports? If so, for which capacity- building supports should these differential price limits be introduced? How should they be calculated? Please provide evidence – for example, if award provisions drive salary costs for specific types of capacity building workers.
Other issues
Are there any other issues with the price limits for capacity building supports?
Plan Management Supports
Current arrangements
Plan Management – Financial Administration funding includes a setup fee to establish the payment arrangements with providers and a monthly processing fee. This support assists a participant by:
Giving increased control over plan implementation and utilisation with plan financial assistance
A Plan Management – Financial Administration provider will possess bookkeeping / accounting skills and qualifications. They will have systems in place for efficiently processing payments on behalf of a participant.
Capacity Building and Training in Plan and Financial Management by a Plan Manager
Develop self-management capabilities
Plan and Financial Capacity Building providers are expected to assist the participant to develop their skills for self-management in future plans, where this is possible. As a part of this capacity building support, providers are to assist the participant to build capacity in the overall management of the plan including engaging providers, developing service agreements, paying providers and claiming payment from the NDIA and maintain records.
Currently, plan mangers are not permitted to claim for provider travel and non-face-to-face activities with respect to support item 14_031_0127_8_3. They are permitted to claim for short notice cancellations.
Issues
Stakeholders have raised a number of issues with the current arrangements, including:
Whether plan managers should be able to claim for provider travel and non-face-to-face activities with respect to support item 14_031_0127_8_3, with the agreement of the participant?
The Annual Price Review 2020-21 is seeking the views of stakeholders on these issues and on any other issues that stakeholders wish to raise.
Is the current price limit for the monthly fee for the ongoing maintenance of the financial management arrangements appropriate? If no, why not? Please provide evidence of the labour and non-labour costs plan management providers face in providing this service.
Is a fixed monthly service fee the best pricing structure? Would it be better for the monthly service fee to be related to the number of transactions made on behalf of a participant or the value of those transactions?
Do the current indexation arrangements for the price limits for plan management supports appropriately maintain their value? If not, what is the appropriate way to reset the price limits on these fees each year in order to maintain their value?
Provider travel and non-face-to-face activities
Classifying Regional, Remote and Very Remote
Current arrangements
The National Disability Insurance Agency (NDIA) uses the 2015 version of the Modified Monash Model (MMM2015) to determine regional, remote and very remote areas. MMM2015 classified areas are based on a scale that is principally concerned with the distance from the area to the nearest population centre and the size of that population centre (see Table below).
| Description | Zones | MMM | Inclusion |
|---|---|---|---|
| Metropolitan | MMM1-3 | 1 | All areas categorised as Major Cities of Australia. |
| Regional Centres | MMM1-3 | 2 | Areas categorised as Inner Regional Australia or Outer Regional Australia that are in, or within 20km road distance, of a town with population >50,000. |
| Regional Centres | MMM1-3 | 3 | Areas categorised as Inner Regional Australia or Outer Regional Australia that are not in MMM 2 and are in, or within 15km road distance, of a town with population between 15,000 and 50,000. |
| Regional Areas | MMM4-5 | 4 | Areas categorised as Inner Regional Australia or Outer Regional Australia that are not in MMM 2 or MMM 3, and are in, or within 10km road distance, of a town with population between 5,000 and 15,000. |
| Regional Areas | MMM4-5 | 5 | All other areas in Inner Regional Australia or Outer Regional Australia. |
| Remote | MMM6 | 6 | All areas categorised Remote Australia that are not on a populated island that is separated from the mainland and is more than 5km offshore. |
| Very Remote | MMM7 | 7 | All other areas – that being Very Remote Australia and areas on a populated island that is separated from the mainland in the ABS geography and is more than 5km offshore. |
Providers and participants can determine the MMM rating of a location using the Health Workforce Locator tool on the Department of Health’s website.
Isolated Towns
Issues
A number of locations have different MMM classifications under the MMM2015 and the MMM2019 systems. This is because some labour supply centres have changed size, and so areas are now closer to or further from the nearest labour supply centre of a given size. It is also because, islands (not connected to the mainland by a bridge) that have an MMM5 classification and that have a population of less than 1,000 are classified as MMM6 under the new MMM2019.
The following Table provides details of the Urban Centres and Localities that will change classification between MMM2015 and MMM2019 to such an extent that the loading that the NDIS applies for planning and price control purposes will be affected. Note, however, that some of these locations would be eligible to be classified as remote under the isolated town policy.
| State | Urban Centres and Localities | MMM2015 | MMM2019 | MMM2015 Loading |
MMM2019 Loading |
MMM2019 Loading (Isolated Towns) |
|---|---|---|---|---|---|---|
| NSW | Bourke | 7 | 6 | 50% | 40% | 40% |
| NSW | Cobar | 7 | 6 | 50% | 40% | 40% |
| NSW | Dangar Island | 5 | 6 | 0% | 40% | 40% |
| Vic | Hopetoun | 6 | 5 | 40% | 0% | 0% |
| Qld | Arcadia Bay, Magnetic Island | 7 | 5 | 50% | 0% | 0% |
| Qld | Cardwell | 6 | 5 | 40% | 0% | 40% |
| Qld | Coochiemudlo Island | 5 | 6 | 0% | 40% | 40% |
| Qld | Duaringa | 6 | 5 | 40% | 0% | 40% |
| Qld | Dunwich | 5 | 6 | 0% | 40% | 40% |
| Qld | Glenden | 5 | 6 | 0% | 40% | 40% |
| Qld | Hideaway Bay - Dingo Beach | 6 | 5 | 40% | 0% | 0% |
| Qld | Horseshoe Bay, Magnetic Island | 7 | 5 | 50% | 0% | 0% |
| Qld | Injune | 7 | 6 | 50% | 40% | 40% |
| Qld | Karragarra Island | 5 | 6 | 0% | 40% | 40% |
| Qld | Lamb Island | 5 | 6 | 0% | 40% | 40% |
| Qld | Nebo | 6 | 5 | 40% | 0% | 0% |
| Qld | Nelly Bay, Magnetic Island | 7 | 5 | 50% | 0% | 0% |
| Qld | Picnic Bay, Magnetic Island | 7 | 5 | 50% | 0% | 0% |
| SA | Penneshaw | 6 | 7 | 40% | 50% | 50% |
| WA | Broome | 7 | 6 | 50% | 40% | 40% |
| WA | Carnarvon | 6 | 7 | 40% | 50% | 50% |
| WA | Green Head | 6 | 5 | 40% | 0% | 0% |
| WA | Kununurra | 6 | 7 | 40% | 50% | 50% |
| WA | Leeman | 6 | 5 | 40% | 0% | 40% |
| NT | Gunbalanya (Oenpelli) | 7 | 6 | 50% | 40% | 40% |
What transitional arrangements, if any, should be put in place for locations that are currently classified as remote under MMM2015 and would no longer be classified as remote under MMM2019?
Are there any other issues with the geographic classification system used by the NDIS for pricing and planning purposes?
Costs in outer regional areas
Current arrangements
Issues
Are the costs of delivering supports in outer regional areas higher than in metropolitan areas? If Yes, why and by how much? Please provide evidence.
If you consider that price limits and plan funding amounts need to be raised in outer regional areas what would be an appropriate loading to cover the additional costs? (A broad range estimate is sufficient). What is the basis of your estimate?
Cancellation rules
Current arrangements
A cancellation is a short notice cancellation if the participant:
does not show up for a scheduled support within a reasonable time, or is not present at the agreed place and within a reasonable time when the provider is travelling to deliver the support; or
Claims for a short notice cancellation should made using the same support item as would have been used if the support had been delivered, using the “Cancellation” option in the myplace portal. When making a claim for a cancelled support the provider should claim for the full-agreed price of the support and indicate in the payment system that the claim is for a cancellation. The payment system will reduce the claim to 90% of the full-agreed price.
There is no limit on the number of short notice cancellations (or no shows) that a provider can claim in respect of a participant. However, providers have a duty of care to their participants and if a participant has an unusual number of cancellations then the provider should seek to understand why they are occurring.
Issues
The Annual Price Review 2020-21 is seeking the views of stakeholders on these issues and on any other issues with cancellations that stakeholders may wish to raise.
9. GUIDE QUESTIONS
What level of administration is involved in replacing a short notice cancellation? What is considered to be appropriate steps in following up and contacting a participant?
What are some of the challenges for participants and their representatives in providing two business days’ notice for a cancellation? For example, falling ill on the day of an appointment?
Provider travel rules
Current arrangements
the Support Catalogue indicates that providers can claim for Provider Travel in respect of that support item;
the provider has the agreement of the participant in advance (i.e. the service agreement between the participant and provider should specify the travel costs that can be claimed); and
Claims for travel in respect of a support must be made separately to the claim for the primary support (the support for which the travel is necessary) using the same line item as the primary support and the “Provider Travel” option in the myplace portal. When claiming for travel in respect of a support, a provider should use the same hourly rate as they have agreed with the participant for the primary support (or a lower hourly rate for the travel if that is what they have agreed with the participant) in calculating the claimable travel cost.
Issues
Stakeholders have raised a number of issues with the current arrangements, including:
Provider travel time limits
What proportion of travel episodes related to the delivery of NDIS supports by your organisation exceed the claimable time limits specified in the NDIS Price Guide and Support Catalogue? Please provide evidence.
On average, what additional non-labour costs per kilometre travelled do you incur because of provider travel? Please provide evidence.
Does the additional cost per kilometre depend on the type of vehicle or other factors? If so, please provide more details? Please provide evidence.
Establishment fees
Current arrangements
The NDIS Price Guide and Support Catalogue currently says:
[The Establishment Fee arrangements apply] to all new NDIS participants in their first plan where they receive at least 20 hours of personal care/community access support per month. This payment is to cover non-ongoing costs for providers establishing arrangements and assisting participants in implementing their plan.
If the participant is choosing to change providers, then the new provider can charge a maximum of $250 against the participant’s plan to assist the participant in changing providers.
Issues
Stakeholders have raised a number of issues with the current price control arrangements for establishment fees, including:
Whether other types of providers should be able to charge an establishment fee?
The Annual Price Review 2020-21 is seeking the views of stakeholders on these issues and on any other issues with the price control arrangements for establishment fees that stakeholders wish to raise.
Are the current price limits for establishment fees appropriate? If no, why not? Please provide evidence of the costs providers face in establishing supports for new clients.
Indexation
